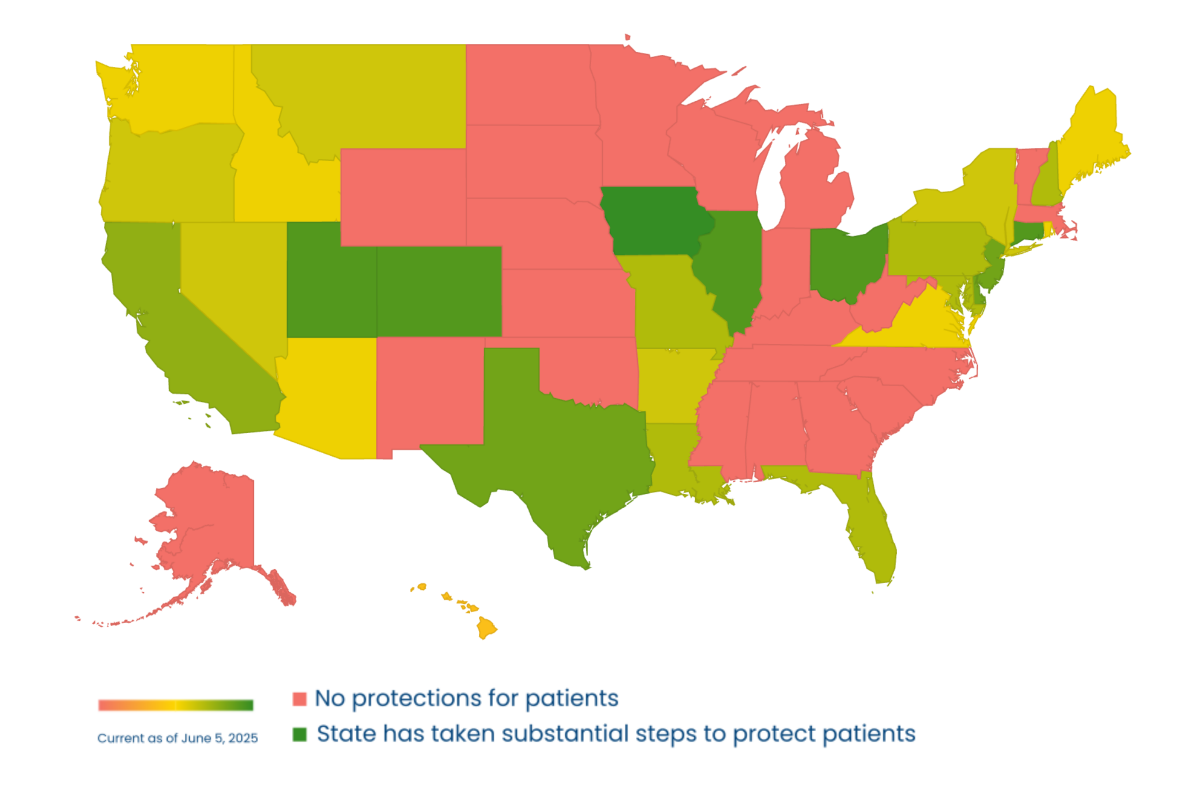
The table below lists states and the status of their laws related to Nonconsensual Practice Pelvic Exams. A state coded “red” does not have laws regulating these practices. A state-coded “green” has passed laws that provide substantial protections for patients.
Nearly every state that has passed a law can improve the law to provide more protections.
Explore the laws in your state and read our recommendations below on how to improve protections for survivors.
Protect Against Nonconsensual Practice Pelvic Exams:
RAINN's Recommendations for Effective State Legislation
A patient drifts into anesthesia for their shoulder surgery. While they're unconscious, a medical student is brought in and asked to practice a pelvic exam on them. The student hesitates - they don’t know the patient, they haven’t discussed the exam - but the pressures of their education wins out and they conduct the non-medically necessary exam. Later, when the patient wakes up, their shoulder hurts - but their genitals are also sore. There’s no record of an exam, they never knew someone would touch them in that intimate place while they were unconscious. The patient leaves, feeling violated and reconsidering future medical care.
This is based on the real experiences of patients and medical students who have testified nationwide on legislation requiring informed consent prior to practicing pelvic exams. Over half the nation now requires informed consent from patients in these settings, protecting students and promoting best practice. The work continues to ensure no one wakes up from an unrelated procedure feeling violated, and no more survivors avoid needed medical care out of fear of a nonconsensual exam. State lawmakers can protect survivors by ensuring their state laws require informed consent before invasive practice exams and hold those who fail to adhere to this best practice accountable.
The Problem
A pelvic exam is a medical procedure in which a healthcare provider examines a person's rectum and/or a woman's reproductive organs, including the vagina, cervix, uterus, and ovaries. This examination is typically conducted for various medical reasons, such as routine screenings, gynecological issues, or during pregnancy.
Informed consent is a fundamental principle in medical ethics, and it involves providing patients with information about a proposed medical procedure, including its purpose, potential risks and benefits, and alternative options so that the patient can make an informed decision about whether to proceed.
Involuntary pelvic exams refer to pelvic examinations that are performed without the explicit and informed consent of the patient. Students initially learn the pelvic examination skills on mannequins or nonpatient volunteers. In an operating room, students can perform this exam while a patient is under anesthesia. In this scenario, nearly half the states allow physicians and medical residents to perform pelvic exams on unconscious patients during unrelated operations without receiving their informed consent. Such an exam amounts to sexual assault on the patient since it has no medical benefit and is performed without their awareness or permission.
Potential harm from this unauthorized exam includes students feeling anxiety and guilt, a patient feeling violated, survivors of sexual assault experiencing post-traumatic stress disorder, and a loss of trust between the patient and their healthcare providers. As one medical student, testifying to a bill requiring informed consent in Ohio, said,
“Our oath as medical students and physicians is to do no harm to the patient. Performing unauthorized pelvic exams on anesthetized patients for the sole purpose of medical student education violates this principle and may cause unacceptable psychological harm to patients. No learning opportunity is worth sacrificing a patient’s wellbeing.”
States have the opportunity to significantly shape the way consent is prioritized for patients in a healthcare setting. Requiring informed consent for practice pelvic exams will improve the quality of every patient's experience with the medical field and maintain a person’s agency over their body during medical interactions. Especially for survivors of sexual assault, ensuring that medical interactions are transparent and safe protects against retraumatization and avoidance of needed healthcare from fear. Transparency cannot occur without both the comfort and consent of patients and medical trainees. Requiring explicit consent for all patients will improve the physician-patient relationship and a patient's psychological and emotional well-being.
Protecting the Patient and Physician Relationship
The physician-patient relationship is built on a foundation of trust. RAINN has heard from survivors regarding unauthorized pelvic exams on patients, despite many medical institutions publicly stating they do not allow the practice. It has long been standard practice not to obtain the patient's consent before conducting the examination.
Many medical students feel as if they cannot opt out of these exams without jeopardizing their grades and careers, since they are conducted under the supervision of residents and attending physicians who write their evaluations. 90% of American medical students in a recent survey stated that they had performed a medical exam on an anesthetized patient. 61% of medical students who had performed a pelvic exam on an anesthetized patient reported doing so without the patient’s explicit consent. Given that many of these students were in schools where involuntary pelvic exams were outlawed, it’s likely that in states that still allow the practice, the percentages are even higher. A later study at the University of Oklahoma found that a large majority of medical students there had performed pelvic exams on gynecological surgery patients and that nearly 75% of these women had not consented to the exam. Legislation and outside oversight are necessary to safeguard patients' rights.
Only 19% of patients reported awareness that medical students might perform pelvic examinations on them during surgery, according to one 2010 study. Furthermore, 72% of women expect to be asked for permission before an exam under anesthesia (EUA), and 62% say they would consent if they were asked.
In recent years, lawmakers, medical students, survivors, and advocates have raised awareness for the rights of patients to be informed and give consent for all medical procedures, including pelvic exams. The American College of Obstetricians and Gynecologists (ACOG) supports explicit informed consent policies. As of now, at least 26 states have passed laws banning unauthorized pelvic exams to ensure transparency and consent is prioritized for all patients, including Illinois, Maryland, Delaware, Pennsylvania, New York, Rhode Island, Connecticut, Maine, Colorado, California, Oregon, Idaho, Florida, Virginia, Arkansas, and Arizona.
A Wisconsin teacher who was given an unauthorized pelvic exam stated that “a woman unconscious on an operating table is at her most vulnerable. If anyone is going to be penetrating…that needs to be disclosed.” And as another survivor stated, “They might not be performing a sexual act, but the result from the patient’s end, from my end, was a feeling of sexual violation.” Creating a universally employed consent process paves the way for all patients' awareness of their bodies to be prioritized when it comes to all pelvic exams, such as prostate, urogenital, and rectal exams.
Informed Consent in the Law and U.S. Dept. of Health and Human Services Guidance
The U.S. Department of Health and Human Services (HHS) issued a memorandum in 2024 addressing involuntary pelvic exams. No federal law exists criminalizing the practice and regulation of the medical field is left primarily to the states, which means state legislation is needed to protect survivors and ensure informed consent practice. In fact, in disseminating the rule, HHS commended states for passing legislation on this issue.
The HHS guidance reinforced informed consent obligations for medical providers, the consequence of which may be loss of funding for the institution itself. If anything, the informed consent obligation sets a standard that state legislatures need to meet or come into alignment with. However, the guidance from HHS only applies in the context of funding under Medicare or Medicaid services. HHS cannot declare involuntary pelvic exams for what they are, which is a crime of sexual assault. State laws can and should mandate informed consent both under physician licensing and oversight, as well as through criminal punishment.
By taking these actions, states can provide protection and support for victims that the guidance from HHS cannot do (for example, they can't get a criminal protective order through a court case). Nothing in the current HHS rules or current guidance requires the loss of a medical license or imposes punishment if a physician were found to have engaged in involuntary pelvic exams (most criminal convictions would impact the medical licensure). Further, current HHS rules and guidance do not provide a voice for victims, because there is no mechanism for investigation by medical licensing organizations or law enforcement. This may result in decreased reporting by survivors.
The HHS guidance reaffirms the requirement for informed consent in these situations as best practice. It carries no legal consequences nor addresses the issue entirely. It sets an expectation for health professionals to follow without truly enforcing the expectation (especially when medical facilities already assure that their policies cover this issue). We hope that legislators addressing this issue will work with hospitals and medical professionals to ensure that informed consent becomes the state policy both in best practices and legal requirements.
RAINN’s Recommendations
RAINN recommends the following to policymakers to ensure state statutes require informed consent by patients, which maintains trust in medical providers and reinforces a bedrock principle of the medical practice to do no harm.
We recognize that each state's code is unique and complicated. RAINN's policy department can work hand-in-hand with lawmakers and their staff to tailor these recommendations to meet each state's specific needs.
-
All practice intimate examinations should require consent.
-
Any healthcare professional or a person under their supervision should be required to obtain informed consent prior to conducting or supervising any practice intimate examination.
-
Consent should be obtained prior to any practice intimate exam in which the patient will be unable to respond at the time of the exam.
-
A description of the practice intimate exam and the patient’s consent to that exam should be in writing and in a document separate from the documents for the medical procedure to ensure the consent is given knowingly.
-
Any exceptions should be limited to medically necessary exams and emergencies.
-
A violation should be considered professional misconduct, and subject to disciplinary action.
All practice intimate examinations should be covered
The type of examination covered should be inclusive of all patients and recognize that any practice intimate examinations are harmful without consent.
Sample Statutory Language:
“Intimate examination” means the performance of a breast, pelvic, anal, rectal, prostate, or other urogenital examination
Any healthcare professional or a person under their supervision should be required to obtain informed consent prior to conducting or supervising any practice intimate examination
Legislation should focus on the consent of the patient because of the harm caused by these practice intimate examinations when the patient does not consent. Any person who either conducts the exam themselves or supervises another person who is conducting the exam, should be included. Occupations to consider include physician, osteopathic physician, surgeon, physician assistant, nurse practitioner, registered nurse, midwife, or emergency medical service personnel. Persons who may be supervised include students, residents, interns, or fellows. Hospitals and medical facilities that knowingly encourage involuntary practice intimate examinations should also be covered by the statute.
Sample Statutory Language:
“Healthcare professional” means a person who is licensed, certified, registered, or otherwise authorized by the laws of this state to administer health care in the ordinary course of the practice of their profession.
“Student” means any person enrolled in a health education program, including in a residency, internship, or fellowship, and is working under the supervision of a healthcare professional.
Consent should be obtained prior to any practice intimate exam in which the patient will be unable to respond at the time of the exam
Patients who are physically incapable of consenting at the time of the exam are especially vulnerable and need to be protected. The harms that can come with these examinations are not only physical harm, but also emotional harm. Victims become distrustful of health care professionals and avoid necessary treatment. A definition should encompass those situations that render a patient physically helpless to object to the medically unnecessary exam.
Sample Statutory Language:
“A healthcare professional or student may not perform or supervise the performance of any intimate examination on a patient who is sedated, anesthetized, or unconscious …”
A description of the practice intimate exam and the patient’s consent to that exam should be in writing and in a document separate from the documents for the medical procedure to ensure the consent is given knowingly
Informed consent is the cornerstone of the medical profession and RAINN’s mission to protect and support survivors. Intimate examinations should only be performed with the informed consent of the patient. To ensure informed consent, a separate notice informing the patient about the procedure and a written consent for the intimate examination should be required. Patients should be aware that the exam is being conducted for non-medical purposes and who will be performing the examination.
Sample Statutory Language:
To obtain specific written informed consent to perform an intimate examination on a sedated, anesthetized, or unconscious patient, a healthcare professional or student shall
-
Provide the patient or the patient’s representative with a written or electronic document that
-
is provided separately from any other notice or agreement;
-
specifies the nature and purpose of the intimate examination;
-
includes a description of the intimate examination to be performed;
-
states which healthcare professional will be performing or supervising the intimate examination;
-
identifies whether the intimate examination will be performed or observed by a student; and
-
Provides the patient the ability to consent to or decline:
-
The intimate examination to be performed by a healthcare professional;
-
The intimate examination to be performed or observed by a student;
-
Clearly state that refusal to consent to the intimate examination will not affect the medical procedure the patient is scheduled to receive
-
Obtain the signature of the patient or the patient’s representative stating they consent to the intimate examination;
-
Sign the consent form
Any exceptions should be limited to medically necessary exams and emergencies.
Healthcare professionals should be allowed to care for their patients in emergency situations, including medically necessary intimate examinations. Any medically necessary exception for consent to intimate examinations likely already exists in the healthcare code, but if an exception is included in the legislation, it should only occur in an emergency situation and only where the examination is necessary to the patient’s health. If an exception exists where an intimate examination is lawfully performed without the informed consent of the patient, the patient should be notified as soon as possible that the intimate examination was performed.
Sample Statutory Language:
… shall not perform unless:
-
The patient or the patient’s representative has given written informed consent to the intimate examination;
-
The performance of the intimate examination is within the scope and standard of care for the procedure or diagnostic examination to be performed on the patient and the patient or the patient's representative has given informed consent;
-
A medical emergency exists and the intimate examination is medically necessary for diagnosis or treatment of the patient;
-
A court orders performance of the intimate examination
A violation should be considered professional misconduct and subject to disciplinary action
Medical licensing bodies need the ability to take corrective action against healthcare professionals and students who perform intimate examinations without the patient’s informed consent. Statutory language should be specific that the violation is misconduct that is actionable against the licensee. This should be done both in the statute prohibiting the practice and in any statute governing the licensure of the healthcare professional.
Sample Statutory Language:
A healthcare professional or student who violates this section or retaliates against an individual who reports a violation of this section engages in unprofessional conduct as defined in [state statute], commits an act that is grounds for discipline, and is subject to discipline by the appropriate licensing board or medical education program pursuant to [insert statutory reference]
AND
The following acts constitute grounds for denial of a license or disciplinary action: …..
(x) performing or supervising the performance of an intimate examination in violation of [state statute]
Model Bill for Intimate Examinations
-
As used in this section:
-
“Healthcare professional” means a person who is licensed, certified, registered, or otherwise authorized by the laws of this state to administer health care in the ordinary course of the practice of their profession.
-
“Intimate examination” means the performance of a breast, pelvic, anal, rectal, prostate, or other urogenital examination
-
“Student” means any person enrolled in a health education program, including in a residency, internship, or fellowship, and is working under the supervision of a healthcare professional.
-
A healthcare professional or student may not perform or supervise the performance of any intimate examination on a patient who is sedated, anesthetized, or unconscious unless:
-
The patient or the patient’s representative has given specific written informed consent to the intimate examination under subsection (3);
-
The performance of the intimate examination is within the scope and standard of care for the procedure or diagnostic examination to be performed on the patient and the patient or the patient's representative has given informed consent;
-
A medical emergency exists and the intimate examination is medically necessary for diagnosis or treatment of the patient;
-
A court orders performance of the intimate examination for collection of evidence;
-
Nothing in this section affects the ability to perform a medical forensic examination, including the collection of evidence, in connection with an alleged sexual assault or other crime or the investigation of an alleged sexual assault or other crime, pursuant to applicable laws.
-
To obtain specific written informed consent to perform an intimate examination on a sedated, anesthetized, or unconscious patient, a healthcare professional or student shall
-
Provide the patient or the patient’s representative with a written or electronic document that
-
is provided separately from any other notice or agreement;
-
specifies the nature and purpose of the intimate examination;
-
includes a description of the intimate examination to be performed;
-
states which healthcare professional will be performing or supervising the intimate examination;
-
identifies whether the intimate examination will be performed or observed by a student; and
-
provides the patient the ability to consent to or decline:
-
the intimate examination to be performed by a healthcare professional; or
-
the intimate examination to be performed by a student;
-
Clearly state that refusal to consent to the intimate examination will not affect the medical procedure the patient is scheduled to receive
-
Obtain the signature of the patient or the patient’s representative stating they consent to the intimate examination; and
-
Sign the consent form
-
If an intimate examination is performed on a sedated, anesthetized, or unconscious patient by a healthcare professional or a student under subdivisions (2)(a)-(e) of this section, the healthcare professional or student shall notify the patient at a reasonable time before the patient is discharged from the care of the healthcare professional.
-
Nothing in this section diminishes any other requirement to obtain informed consent for an intimate examination or any other procedure
-
A healthcare professional or student who violates this section or retaliates against an individual who reports a violation of this section engages in unprofessional conduct as defined in [state statute], commits an act that is grounds for discipline, and is subject to discipline by the appropriate licensing board or medical education program pursuant to [insert statutory reference]
[Separate statutory language in misconduct statute] The following acts constitute grounds for denial of a license or disciplinary action: …..
(x) performing or supervising the performance of an intimate examination in violation of [state statute]
Next Steps:
For more information about the laws in your state, please see RAINN's state law database. For additional information about involuntary pelvic exams generally, please visit RAINN's website. To schedule a call with someone on RAINN’s policy team, email policy@rainn.org.